Avastin抑制兔眼小梁切除术后滤过泡瘢痕化的作用
热度0票 浏览78次
时间:2011年3月05日 11:15
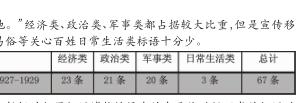
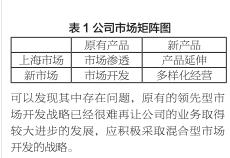
【摘要】 目的:探讨Avastin抑制兔眼小梁切除术后滤过泡纤维瘢痕形成的作用。方法:兔20只40眼随机分为3个不同剂量Avastin实验组、丝裂霉素 C(MMC)对照组及空白对照组。对兔眼行常规小梁切除术,Avastin实验组于术毕及术后3,7d术区结膜下分别注射0.5,1及2mg Avastin;MMC对照组术中筋膜囊、巩膜瓣下放置0.2g/L MMC棉片。术后裂隙灯下观察滤过泡形态及角膜、前房等情况;术后7,14d摘除眼球,常规HE染色观察组织形态,在高倍视野中,通过滤过泡腔面在结膜中形成的面积百分比及滤过泡形成区在结膜中面积百分比,评价不同剂量Avastin结膜下注射对滤过泡形成及纤维化的影响。结果:术后7d各组结膜纤维结缔组织中均可见明显的滤过泡形成。术后14d仅注射2mg Avastin实验组及MMC对照组的结膜组织中可见明显滤过泡;1mg Avastin实验组见少量面积微小的滤过泡;0.5mg Avastin实验组及空白对照组滤过泡均消失,纤维组织增生明显。术后7d各组高倍视野下滤过泡腔面在结膜中形成的面积百分比及滤过泡形成区在结膜中面积百分比无明显差异。术后14d,2mg及1mg Avastin实验组滤过泡腔面积在结膜中形成的面积百分比分别为1.0%,0.8%,MMC组为0.9%。2mg及1mg Avastin实验组滤过泡形成区在结膜中面积百分比分别为26.1%,2.9%,MMC组为25.8%。2mg及1mg Avastin实验组的滤过泡腔面及形成区面积与结膜面积的百分比均明显高于空白对照组,单项方差分析结果分别为 F=270.10,P=0.00;F=49.99,P=0.00;2mg Avastin实验组的上述滤过泡面积百分比与MMC组无差异。结论:结膜下注射Avastin可有效帮助滤过术后滤过泡的形成与维持,缓解滤过泡的纤维增生。教师职称论文发表
【关键词】 Avastin;滤过泡;瘢痕化;小梁切除术;血管内皮生长因子
Abstract?AIM: To evaluate the efficacy of Avastin on treating the bleb fibrosis after trabeculectomy in rabbits. METHODS: Forty eyes of 20 rabbits undergone trabeculectomy were randomly divided into three different doses of Avastin experimental groups, mitomycin C(MMC)group and blank control group. The eyes in three Avastin experimental groups were randomly received subconjunctival injection of 0.5,1,2mg Avastin when trabeculectomy finished and on 3rd,7th days after surgery. In the MMC treated group,MMC cotton patch,0.2g/L, was put under the capsule Tenons and scleral flap during operation. The appearance of filtrating bleb and inflammatory reactions were observed under slit?lamp; the filter areas were taken histopathologic examination on postoperative 7,14 days. RESULTS: Filter blebs could be seen clearly in each group on postoperative 7 days. And on postoperative 14 days in the 2mg Avastin group and MMC group, filtering blebs were larger and more elevated than other groups; in 1mg Avastin group, there were only some small blebs; and in 0.5mg Avastin group and blank control group, filter blebs disappeared, and marked hyperplasia of fibrous tissue could be seen. Under the microscope on postoperative 7 days, there was no significant difference in the percentage of the bleb cavity surface area in the conjunctiva and the percentage of bleb?forming region in the conjunctiva. On postoperative 14 days, the percentage of the bleb cavity surface area in the conjunctiva of 2 mg and 1mg Avastin groups and MMC group were respectively 1.0%, 0.8%, 0.9%;and the percentage of bleb?forming region in the conjunctiva were 26.1%, 2.9%, 25.8%. The percentage of the bleb cavity surface area in the conjunctiva and the percentage of bleb?forming region in the conjunctiva of 2mg and 1 mg Avastin group were significantly higher than the blank control group, respectively(P=0.00; P=0.00). But there was no significantly difference between 2mg Avastin group and MMC group on the filtering bleb area percentage. CONCLUSION: Subconjunctival injection of Avastin can effectively prevent the bleb fibrosis, maintain larger bleb area. This indicates that Avastin is most likely to be a novel agent to prevent excessive scarring following trabeculectomy.
?
KEYWORDS:Avastin;filter bleb;fibrosis;trabeculectomy; vascular endothelial growth factor
0 引言教师职称论文发表
小梁切除术是青光眼的主要治疗手段,常常因滤过泡的瘢痕化导致手术失败。现代抗代谢药物仍存在一定的缺陷及并发症,限制了其临床应用。近年研究发现,组织创伤愈合过程中会伴有血管内皮生长因子(vascular endothelial growth factor,VEGF)释放增加,从而促进纤维瘢痕组织增生[1]。因此,我们通过结膜下注射Avastin抑制VEGF的作用,进而抑制纤维组织增生,减轻兔眼小梁切除术后滤过泡纤维瘢痕形成如下。
1 材料和方法
1.1 材料
健康成年新西兰白兔20只,体质量2.0~2.5kg,广东省动物实验中心提供;Avastin(香港九龙药业),丝裂霉素C(MMC,日本协和发酵工业株式会社),手术显微镜(德国Zeiss)。
1.2 方法
新西兰白兔20只40眼随机分为0.5,1,2mg Avastin实验组、丝裂霉素C对照组、空白对照组,每组8眼。3g/L戊巴比妥钠按照1mL/kg im麻醉实验兔,行常规小梁切除术。Avastin实验组分别于术毕及术后3,7d结膜下注射0.5,1,2mg Avastin;MMC组术中用浸有0.2g/L的MMC棉片置于筋膜囊、巩膜瓣下3min,然后用生理盐水180mL反复冲洗术区。空白对照组行常规手术后不进行其他处理。
1.2.1 裂隙灯观察
术后每天裂隙灯下观察滤过泡形态,角膜及前房反应等情况。滤过泡分为功能型及非功能型:功能型为扁平/隆起弥散型,非功能型为局部充血包裹/不形成滤过泡。
1.2.2 病理学检查
于术后7,14d每组随机摘取4眼,取滤过泡及其周围的结膜、巩膜全层球壁组织8mm×6mm,置于40g/L甲醛固定,常规脱水,石蜡包埋,每隔0.5mm连续切片5张,行HE染色,中性树胶封片后显微镜下观察。利用病理图像分析系统测量每组10个高倍视野中滤过泡腔面积、滤过泡形成区面积及视野中结膜面积。计算:滤过泡腔面在结膜中形成的面积百分比=(滤过泡腔面积/结膜面积)×100%;滤过泡形成区在结膜中面积百分比=(滤过泡形成区面积/结膜面积)×100%。教师职称论文发表
统计学分析:利用SPSS 18.0软件处理数据,各组术后不同时间点面积百分比的比较采用单因素的方差分析,以评价不同剂量Avastin结膜下注射对滤过泡形成及纤维化的影响。P<0.05为差异有统计学意义。
2 结果
2.1 裂隙灯下观察
术后1d各组均形成功能性滤过泡,伴有不同程度充血,3d后充血逐渐减轻。术后7d,Avastin实验组与MMC对照组滤过泡隆起弥散,表面血管稀疏;空白对照组术后3d滤过泡开始局限化,至7d滤过泡周围可见粗大血管。术后14d,1,2mg Avastin实验组与MMC对照组滤过泡扁平弥散,血管稀疏纤细;0.5mg Avastin实验组滤过泡血管包裹局限;空白对照组滤过泡瘢痕化、表面血管粗大。术后1d所有术眼均有不同程度前房渗出,但均于5d内吸收;部分前房少许积血,7d内自行吸收。未见角膜水肿、上皮脱失、浅前房及滤过泡渗漏等并发症。
2.2 组织学检查
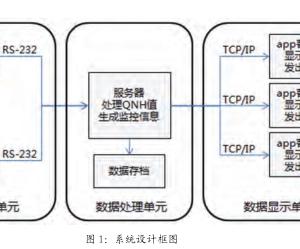
术后7d,各实验组及对照组均可见明显滤过泡结构,纤维组织轻度增殖(图1A);MMC组结膜下及角巩膜缘可见大量炎症细胞(图1B)。术后 14d,2mg Avastin实验组与MMC对照组仍可见明显滤过泡囊腔结构,纤维组织增生(图1C);1mg Avastin实验组滤过泡微小,纤维组织增生明显(图1D);0.5mg Avastin实验组与空白对照组可见大量纤维组织增生,未见滤过泡(图1E)。术后7d,各组高倍视野下滤过泡腔面在结膜中形成的面积百分比及滤过泡形成区在结膜中面积百分比无明显差异。术后14d,2mg及1mg Avastin实验组滤过泡腔面在结膜中形成的平均面积百分比分别为1.0%±0.1%,0.8%±0.1%,MMC组为0.9%±0.1%;2mg及 1mg Avastin实验组滤过泡形成区在结膜中平均面积百分比分别为26.1%±6.2%,2.9%±0.3%,MMC组为25.8%±5.1%。2mg及 1mg Avastin的实验组滤过泡腔面面积及形成区面积与结膜面积的百分比均明显高于空白对照组,单因素方差分析结果分别为 F=270.10,P=0.00;F=49.99,P=0.00。2mg Avastin实验组的上述滤过泡面积百分比与MMC组无差异。
3 讨论
小梁切除术是目前治疗青光眼的主要手术方法,但术后滤过泡的瘢痕化常常导致手术失败。虽然抗代谢药物(如MMC,5?Fu,环孢素A等)的应用大大提高了手术成功率,但发生低眼压、滤过泡渗漏等并发症的风险非常高[2],大大限制了其临床应用。寻求更为安全有效的抗瘢痕化药物成为目前青光眼治疗研究中的一大热点。Avastin 是全长的人源化单克隆抗体,可与VEGF的所有异构体结合抑制新生血管的生成。Michels等[3]首先报道了玻璃体内注射Avastin治疗年龄相关性黄斑变性的新生血管,Kahook等[4]将其应用于治疗新生血管性青光眼亦取得了良好的临床效果。动物实验亦显示了Avastin在抗瘢痕化方面的作用[5], Kahook等[6]报道了结膜下注射Avastin使已经瘢痕化滤过泡更为弥散隆起,表面新生血管明显消退,但是关于Avastin防治滤过泡瘢痕化的具体过程及作用进程,目前国内外尚未见类似的研究报道。我们在实验性滤过手术的同时辅助结膜下注射Avastin,探讨Avastin防治滤过泡瘢痕化的作用,希望为青光眼滤过手术的成功提供更大的可能。组织创伤后由含新生血管、成纤维细胞及纤维组织的肉芽组织修复,这一过程涉及了包括VEGF在内的多种生长因子的相互作用。近来研究显示兔眼小梁切除术后会出现VEGF释放增多及Tenon?s囊中成纤维细胞的增生[7]。Tenon?s囊成纤维细胞可产生大量的胶原弹性蛋白,是造成小梁切除术后瘢痕形成的重要原因。我们在小梁切除术后结膜下注射Avastin,通过拮抗VEGF的作用,抑制新生血管生成,减轻新生血管渗漏及胶原沉积;同时抑制VEGF对成纤维细胞的刺激作用,减弱成纤维细胞与炎症细胞间迁移、增殖的级联反应,进而抑制滤过泡的纤维化,促进功能性滤过泡的形成,提高手术成功率。研究显示,结膜下注射Avastin可有效帮助滤过术后滤过泡的形成与维持,缓解滤过泡的纤维增生,2mg的 Avastin的治疗效果与MMC等同,而且术后角膜缘炎症反映明显较轻,可能与Avastin减轻血管渗漏及抑制炎症级联反应有关。
教师职称论文发表
综上所述,在兔眼小梁切除术后结膜下注射Avastin可有效抑制滤过泡的血管炎症反应及纤维增生,促进功能性滤过泡的形成,提高手术成功率。因此Avastin有望成为一种新的抗瘢痕化药物应用于青光眼滤过性手术。
【参考文献】
1 Wilgus TA, Ferreira AM, Oberyszyn TM, et al. Regulation of scar formation by vascular endothelial growth factor. Lab Invest 2008;88(6):579?590
2 Lama PJ, Fechtner RD. Antifibrotic and wound healing in glaucoma surgery. Surv Ophthalmol 2003;48(3):314?346
3 Michels S, Rosenfeld PJ, Puliafito CA, et al. Systemic bevacizumab (Avastin) therapy for neovascular age?related macular degeneration twelve?week results of an uncontrolled open?label clinical study. Ophthalmology 2005;112(6):1035?1047
4 Kahook MY, Schuman JS, Noecker RJ. Intravitreal bevacizumab in a patient with neovascular glaucoma. Ophthalmic Surg Lasers Imaging 2006;37(2):144?146
5 Farnaz M, Rohit V, Le?Tien L, et al. Postoperative use of bevacizumab as an antifibrotic agent in glaucoma filtration surgery in the rabbit. Invest Ophthalmol Vis Sci 2009;50(7):3233?3237
6 Kahook MY,Schuman JS, Robert JN. Needle bleb revision of encapsulated filtering bleb with bevacizumab. Ophthalmic Surg Lasers Imaging 2006;7(2):148?150
7 Li Z, Van Bergen T, Van de Veire S, et al. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci 2009;50:5217?5225教师职称论文发表
【关键词】 Avastin;滤过泡;瘢痕化;小梁切除术;血管内皮生长因子
Abstract?AIM: To evaluate the efficacy of Avastin on treating the bleb fibrosis after trabeculectomy in rabbits. METHODS: Forty eyes of 20 rabbits undergone trabeculectomy were randomly divided into three different doses of Avastin experimental groups, mitomycin C(MMC)group and blank control group. The eyes in three Avastin experimental groups were randomly received subconjunctival injection of 0.5,1,2mg Avastin when trabeculectomy finished and on 3rd,7th days after surgery. In the MMC treated group,MMC cotton patch,0.2g/L, was put under the capsule Tenons and scleral flap during operation. The appearance of filtrating bleb and inflammatory reactions were observed under slit?lamp; the filter areas were taken histopathologic examination on postoperative 7,14 days. RESULTS: Filter blebs could be seen clearly in each group on postoperative 7 days. And on postoperative 14 days in the 2mg Avastin group and MMC group, filtering blebs were larger and more elevated than other groups; in 1mg Avastin group, there were only some small blebs; and in 0.5mg Avastin group and blank control group, filter blebs disappeared, and marked hyperplasia of fibrous tissue could be seen. Under the microscope on postoperative 7 days, there was no significant difference in the percentage of the bleb cavity surface area in the conjunctiva and the percentage of bleb?forming region in the conjunctiva. On postoperative 14 days, the percentage of the bleb cavity surface area in the conjunctiva of 2 mg and 1mg Avastin groups and MMC group were respectively 1.0%, 0.8%, 0.9%;and the percentage of bleb?forming region in the conjunctiva were 26.1%, 2.9%, 25.8%. The percentage of the bleb cavity surface area in the conjunctiva and the percentage of bleb?forming region in the conjunctiva of 2mg and 1 mg Avastin group were significantly higher than the blank control group, respectively(P=0.00; P=0.00). But there was no significantly difference between 2mg Avastin group and MMC group on the filtering bleb area percentage. CONCLUSION: Subconjunctival injection of Avastin can effectively prevent the bleb fibrosis, maintain larger bleb area. This indicates that Avastin is most likely to be a novel agent to prevent excessive scarring following trabeculectomy.
?
KEYWORDS:Avastin;filter bleb;fibrosis;trabeculectomy; vascular endothelial growth factor
0 引言教师职称论文发表
小梁切除术是青光眼的主要治疗手段,常常因滤过泡的瘢痕化导致手术失败。现代抗代谢药物仍存在一定的缺陷及并发症,限制了其临床应用。近年研究发现,组织创伤愈合过程中会伴有血管内皮生长因子(vascular endothelial growth factor,VEGF)释放增加,从而促进纤维瘢痕组织增生[1]。因此,我们通过结膜下注射Avastin抑制VEGF的作用,进而抑制纤维组织增生,减轻兔眼小梁切除术后滤过泡纤维瘢痕形成如下。
1 材料和方法
1.1 材料
健康成年新西兰白兔20只,体质量2.0~2.5kg,广东省动物实验中心提供;Avastin(香港九龙药业),丝裂霉素C(MMC,日本协和发酵工业株式会社),手术显微镜(德国Zeiss)。
1.2 方法
新西兰白兔20只40眼随机分为0.5,1,2mg Avastin实验组、丝裂霉素C对照组、空白对照组,每组8眼。3g/L戊巴比妥钠按照1mL/kg im麻醉实验兔,行常规小梁切除术。Avastin实验组分别于术毕及术后3,7d结膜下注射0.5,1,2mg Avastin;MMC组术中用浸有0.2g/L的MMC棉片置于筋膜囊、巩膜瓣下3min,然后用生理盐水180mL反复冲洗术区。空白对照组行常规手术后不进行其他处理。
1.2.1 裂隙灯观察
术后每天裂隙灯下观察滤过泡形态,角膜及前房反应等情况。滤过泡分为功能型及非功能型:功能型为扁平/隆起弥散型,非功能型为局部充血包裹/不形成滤过泡。
1.2.2 病理学检查
于术后7,14d每组随机摘取4眼,取滤过泡及其周围的结膜、巩膜全层球壁组织8mm×6mm,置于40g/L甲醛固定,常规脱水,石蜡包埋,每隔0.5mm连续切片5张,行HE染色,中性树胶封片后显微镜下观察。利用病理图像分析系统测量每组10个高倍视野中滤过泡腔面积、滤过泡形成区面积及视野中结膜面积。计算:滤过泡腔面在结膜中形成的面积百分比=(滤过泡腔面积/结膜面积)×100%;滤过泡形成区在结膜中面积百分比=(滤过泡形成区面积/结膜面积)×100%。教师职称论文发表
统计学分析:利用SPSS 18.0软件处理数据,各组术后不同时间点面积百分比的比较采用单因素的方差分析,以评价不同剂量Avastin结膜下注射对滤过泡形成及纤维化的影响。P<0.05为差异有统计学意义。
2 结果
2.1 裂隙灯下观察
术后1d各组均形成功能性滤过泡,伴有不同程度充血,3d后充血逐渐减轻。术后7d,Avastin实验组与MMC对照组滤过泡隆起弥散,表面血管稀疏;空白对照组术后3d滤过泡开始局限化,至7d滤过泡周围可见粗大血管。术后14d,1,2mg Avastin实验组与MMC对照组滤过泡扁平弥散,血管稀疏纤细;0.5mg Avastin实验组滤过泡血管包裹局限;空白对照组滤过泡瘢痕化、表面血管粗大。术后1d所有术眼均有不同程度前房渗出,但均于5d内吸收;部分前房少许积血,7d内自行吸收。未见角膜水肿、上皮脱失、浅前房及滤过泡渗漏等并发症。
2.2 组织学检查
术后7d,各实验组及对照组均可见明显滤过泡结构,纤维组织轻度增殖(图1A);MMC组结膜下及角巩膜缘可见大量炎症细胞(图1B)。术后 14d,2mg Avastin实验组与MMC对照组仍可见明显滤过泡囊腔结构,纤维组织增生(图1C);1mg Avastin实验组滤过泡微小,纤维组织增生明显(图1D);0.5mg Avastin实验组与空白对照组可见大量纤维组织增生,未见滤过泡(图1E)。术后7d,各组高倍视野下滤过泡腔面在结膜中形成的面积百分比及滤过泡形成区在结膜中面积百分比无明显差异。术后14d,2mg及1mg Avastin实验组滤过泡腔面在结膜中形成的平均面积百分比分别为1.0%±0.1%,0.8%±0.1%,MMC组为0.9%±0.1%;2mg及 1mg Avastin实验组滤过泡形成区在结膜中平均面积百分比分别为26.1%±6.2%,2.9%±0.3%,MMC组为25.8%±5.1%。2mg及 1mg Avastin的实验组滤过泡腔面面积及形成区面积与结膜面积的百分比均明显高于空白对照组,单因素方差分析结果分别为 F=270.10,P=0.00;F=49.99,P=0.00。2mg Avastin实验组的上述滤过泡面积百分比与MMC组无差异。
3 讨论
小梁切除术是目前治疗青光眼的主要手术方法,但术后滤过泡的瘢痕化常常导致手术失败。虽然抗代谢药物(如MMC,5?Fu,环孢素A等)的应用大大提高了手术成功率,但发生低眼压、滤过泡渗漏等并发症的风险非常高[2],大大限制了其临床应用。寻求更为安全有效的抗瘢痕化药物成为目前青光眼治疗研究中的一大热点。Avastin 是全长的人源化单克隆抗体,可与VEGF的所有异构体结合抑制新生血管的生成。Michels等[3]首先报道了玻璃体内注射Avastin治疗年龄相关性黄斑变性的新生血管,Kahook等[4]将其应用于治疗新生血管性青光眼亦取得了良好的临床效果。动物实验亦显示了Avastin在抗瘢痕化方面的作用[5], Kahook等[6]报道了结膜下注射Avastin使已经瘢痕化滤过泡更为弥散隆起,表面新生血管明显消退,但是关于Avastin防治滤过泡瘢痕化的具体过程及作用进程,目前国内外尚未见类似的研究报道。我们在实验性滤过手术的同时辅助结膜下注射Avastin,探讨Avastin防治滤过泡瘢痕化的作用,希望为青光眼滤过手术的成功提供更大的可能。组织创伤后由含新生血管、成纤维细胞及纤维组织的肉芽组织修复,这一过程涉及了包括VEGF在内的多种生长因子的相互作用。近来研究显示兔眼小梁切除术后会出现VEGF释放增多及Tenon?s囊中成纤维细胞的增生[7]。Tenon?s囊成纤维细胞可产生大量的胶原弹性蛋白,是造成小梁切除术后瘢痕形成的重要原因。我们在小梁切除术后结膜下注射Avastin,通过拮抗VEGF的作用,抑制新生血管生成,减轻新生血管渗漏及胶原沉积;同时抑制VEGF对成纤维细胞的刺激作用,减弱成纤维细胞与炎症细胞间迁移、增殖的级联反应,进而抑制滤过泡的纤维化,促进功能性滤过泡的形成,提高手术成功率。研究显示,结膜下注射Avastin可有效帮助滤过术后滤过泡的形成与维持,缓解滤过泡的纤维增生,2mg的 Avastin的治疗效果与MMC等同,而且术后角膜缘炎症反映明显较轻,可能与Avastin减轻血管渗漏及抑制炎症级联反应有关。
教师职称论文发表
综上所述,在兔眼小梁切除术后结膜下注射Avastin可有效抑制滤过泡的血管炎症反应及纤维增生,促进功能性滤过泡的形成,提高手术成功率。因此Avastin有望成为一种新的抗瘢痕化药物应用于青光眼滤过性手术。
【参考文献】
1 Wilgus TA, Ferreira AM, Oberyszyn TM, et al. Regulation of scar formation by vascular endothelial growth factor. Lab Invest 2008;88(6):579?590
2 Lama PJ, Fechtner RD. Antifibrotic and wound healing in glaucoma surgery. Surv Ophthalmol 2003;48(3):314?346
3 Michels S, Rosenfeld PJ, Puliafito CA, et al. Systemic bevacizumab (Avastin) therapy for neovascular age?related macular degeneration twelve?week results of an uncontrolled open?label clinical study. Ophthalmology 2005;112(6):1035?1047
4 Kahook MY, Schuman JS, Noecker RJ. Intravitreal bevacizumab in a patient with neovascular glaucoma. Ophthalmic Surg Lasers Imaging 2006;37(2):144?146
5 Farnaz M, Rohit V, Le?Tien L, et al. Postoperative use of bevacizumab as an antifibrotic agent in glaucoma filtration surgery in the rabbit. Invest Ophthalmol Vis Sci 2009;50(7):3233?3237
6 Kahook MY,Schuman JS, Robert JN. Needle bleb revision of encapsulated filtering bleb with bevacizumab. Ophthalmic Surg Lasers Imaging 2006;7(2):148?150
7 Li Z, Van Bergen T, Van de Veire S, et al. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci 2009;50:5217?5225教师职称论文发表